| Index to this page |
When blood vessels are cut or damaged, the loss of blood from the system must be stopped before shock and possible death occur. This is accomplished by solidification of the blood, a process called coagulation or clotting.
A blood clot consists ofBy tradition, these factors are designated by Roman numerals. I find this somewhat cumbersome and will use Arabic numerals as well.
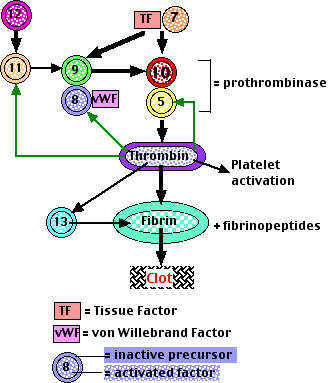 There are two processes that can initiate clotting:
There are two processes that can initiate clotting:
Platelets are cell fragments produced from megakaryocytes.
Blood normally contains 150,000 to 400,000 per microliter (µl). If this value should drop much below 20,000/µl, there is a danger of uncontrolled bleeding. This is because of the essential role of plateletsThese actions cause a plug of platelets to form at the site.
The bound platelets release
ReoPro® is a monoclonal antibody directed against platelet receptors. It inhibits platelet aggregation and appears to reduce the risk that "reamed out" coronary arteries (after coronary angioplasty) will plug up again.
The deficiency may arise because
In some cases of von Willebrand disease, either a deficient level or a mutant version of the factor eliminates its protective effect on factor 8. The resulting low level of factor 8 mimics hemophilia A.
Why do all the human bleeding disorders involve factors in amplification pathways? Probably because they are the only deficiencies that can be tolerated. Loss of the genes forThe genes encoding factors 8 and 9 are on the X chromosome. Thus their inheritance is X-linked.
Like other X-linked disorders, hemophilia A and B are found almost exclusively in males because they inherit just a single X chromosome, and if the gene for factor 8 (or 9) on it is defective, they will suffer from the disease.
Queen Victoria of the UK was a carrier of a mutant factor 9 gene and passed it on to several of her descendants. Link to a discussion and pedigree.
There are many different mutant versions of the genes for factors 8 and 9. Although some produce only a minor effect on the function of their protein, others fail to produce any functioning clotting factor.
Factor 8 and 9 can be extracted from donated blood, usually pooled from several thousand donors, and purified. Injections of this material can halt episodes of bleeding in hemophiliacs and have allowed countless young men to live relatively normal lives.
However, in the early 1980s, blood contaminated with the human immunodeficiency virus (HIV) was unknowingly used to manufacture preparations of factors 8 and 9. In some areas, 90% or more of the hemophiliacs became infected by these contaminated preparations. Many have since died of AIDS.
The future now looks brighter because:These recombinant factors are made by inserting the DNA encoding the human protein into mammalian cells grown in culture [Discussion]. E. coli cannot be used because these factors are glycoproteins, and E. coli lacks the machinery to attach carbohydrate properly.
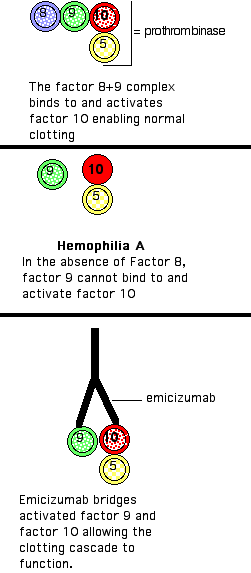
In order for the clotting cascade to work, both factors 8 and 9 are needed to bind to, and thus activate, factor 10 (see above). Patients with hemophilia A have little or no factor 8 and thus the clotting cascade cannot proceed (middle image).
Emicizumab is a monoclonal antibody developed by recombinant DNA technology. Unlike conventional antibodies with two identical binding sites [View], emicizumab is bispecific: that is, one of its arms binds to activated factor 9 (IX), the other to factor 10 (X). This brings the two together so that the clotting cascade can proceed (bottom image).
Phase 3 clinical trials of emicizumab look promising (autumn of 2017).
The 7 December 2017 issue of The New England Journal of Medicine carries a report on a trial of gene therapy in 10 boys with hemophilia B.
The 28 December 2017 issue of The New England Journal of Medicine carries a report of a Phase I/II study of seven men given a single intravenous injection of an AAV vector containing the DNA encoding Factor VIII (the clotting factor that results in hemophilia A if insufficient levels are present).
Read more about these trials at this LINK.
It is difficult to see how even the most worried critics of genetic engineering can fail to approve its potential to save the lives of thousands of hemophiliacs in the years to come.
It does so by binding to and thus inactivating:
Heparin is a mixture of polysaccharides that bind to antithrombin III, inducing an allosteric change that greatly enhances its inhibition of thrombin synthesis. Some surgical patients, especially those receiving hip or heart valve replacements, and people at risk of ischemic stroke (clots in the brain), are given heparin.
With its many clot-promoting activities, it is probably no accident that thrombin sits at the center of the control mechanism.
Recombinant Protein C is now available to treat people threatened with inappropriate clotting, e.g., as a result of widespread infection (sepsis).
Conversely, blocking the action of vitamin K helps to prevent inappropriate clotting.
Warfarin (Coumadin®) is sometimes prescribed as a "blood thinner" because it is an effective vitamin K antagonist. (Warfarin is also used as a rat poison because it can cause lethal internal bleeding.)
Warfarin treatment is tricky because the therapeutic window (neither too much nor too little) is very narrow, and there is substantial variability between people in their response. So treatment requires regular monitoring of clotting time until the proper dosage is established.
However, two new anti-clotting agents — Eliquis® and Xarelto® — are turning out to be safer and effective alternatives to warfarin. They work by inhibiting activated factor 10 (Factor Xa)
Plasma contains plasminogen, which binds to the fibrin molecules in a clot. Nearby healthy cells release tissue plasminogen activator (TPA), which also binds to fibrin and, as its name suggests, activates plasminogen forming plasmin. Plasmin (another serine protease) proceeds to digest fibrin, thus dissolving the clot.
Recombinant human TPA is now produced by recombinant DNA technology. Injected within the first hours after a heart attack, it has saved many lives by dissolving the clot blocking the coronary artery and restoring blood flow before the heart muscle becomes irreversibly damaged. It is also used for people who suffer an ischemic stroke; that is, a clot in the brain. (It must not, of course, be used for hemorrhagic strokes, that is, a burst blood vessel!)
| External Link |
| More details available at: Blood Coagulation |
| Please let me know by e-mail if you find a broken link in my pages.) |
Thrombin (as well as factors 7 and 10) promotes healing by stimulating the growth of new blood vessels at the site of damage. [Link to a discussion of angiogenesis.]
| Welcome&Next Search |